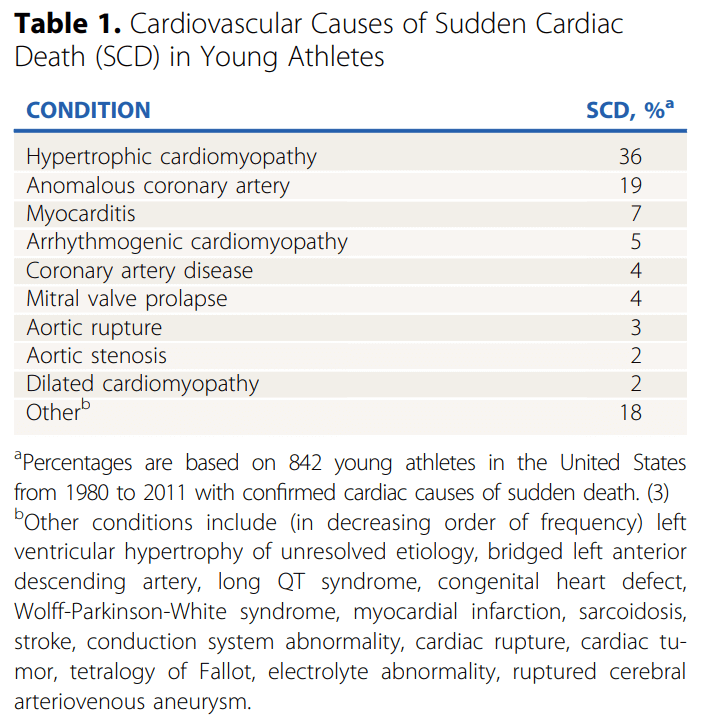
The risk for sudden death in young athletes with cardiovascular disease is 2.5 times higher than that in non-athletes. In fact, over 90% of sudden cardiac death (SCD) occurs during or immediately after a training session or competition, according to a clinical review recently published in the Journal of the American College of Cardiology.
The American Heart Association® (AHA) attributes hypertrophic cardiomyopathy (HCM) as the leading cause of SCD in young athletes. SCD disproportionately affects Black athletes and is more frequently linked to competitive sports that involve sudden movements, such as football or basketball. However, the majority of pediatric patients show no signs or symptoms of HCM prior to experiencing sudden cardiac arrest.
Dr. Robert Spencer is a board-certified pediatric cardiologist at Staten Island University Hospital, Northwell Health, with a special focus on the prevention of sudden cardiac death in young athletes. He serves as the Director of the Pediatric Simulation Program, where he leads educational initiatives to enhance emergency preparedness among pediatric trainees.
We sat down with Dr. Spencer to discuss a research article he co-authored with his colleague, Dr. Shahed Quraishi, regarding athlete screening and sudden cardiac death. This study was published in Pediatrics in Review, an official journal of the American Academy of Pediatrics.
Q: In your research, you discussed several cardiac conditions associated with SCD. Regarding HCM, you referenced the complicated nature of recommendations against participation in competitive sports. What would be the associated risks and benefits of sports participation for a patient with HCM?
Sports participation can be a complex challenge for patients with hypertrophic cardiomyopathy. The primary concern is the risk of sudden cardiac death, which can occur due to exercise-induced arrhythmias, especially in high-intensity sports. Patients with specific risk factors, such as significant left ventricular hypertrophy, a history of syncope, or a family history of sudden death, are at higher risk and require individualized management.
However, participation in physical activity also offers patients important health benefits, including improved cardiovascular fitness, mental well-being, and overall quality of life. Current guidelines emphasize a shared decision-making approach, allowing for individualized discussions between healthcare providers, patients, and their families to assess the risks and benefits. While high-intensity sports are typically discouraged, many patients can safely participate in lower-intensity activities with appropriate monitoring and precautions in place.
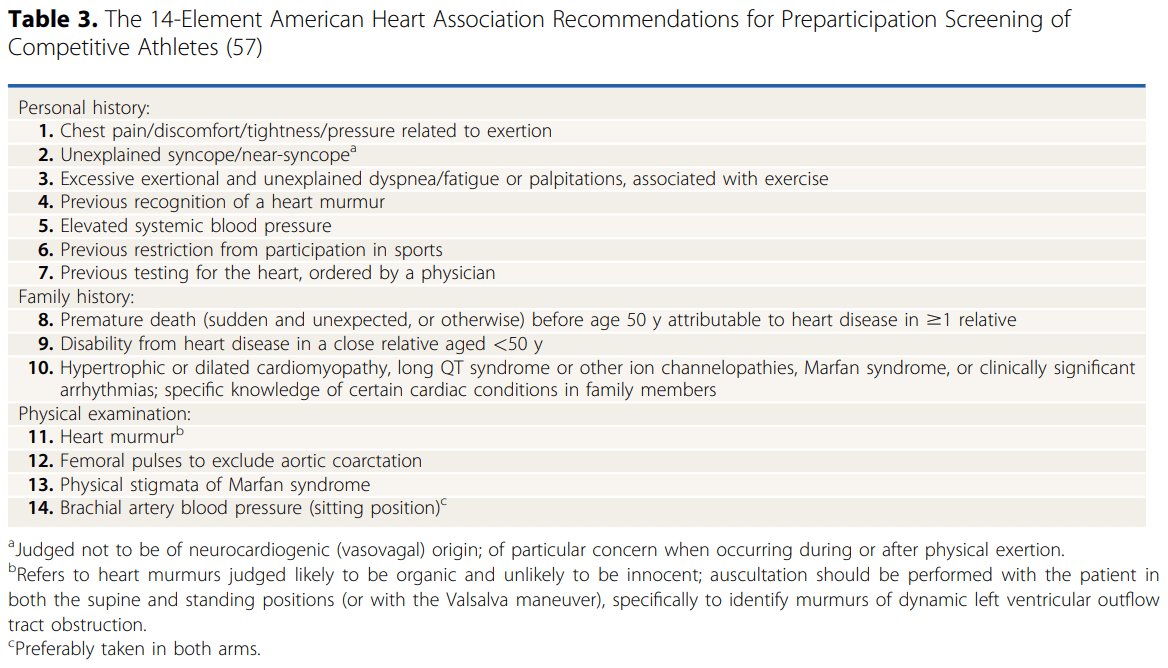
Q: In your study, you discussed the AHA’s 14-element screening tool was ‘heavily underused’ and referenced a recent study that revealed only 27% of 48 participating states utilized all 14 elements in their screening forms. Could you explain the barriers to use of this tool and how providers could overcome such hurdles?
There are several factors that contribute to the inconsistent use of the AHA's 14-element screening tool. A major challenge is a lack of awareness among healthcare providers, many of whom may not fully recognize the importance of comprehensive cardiovascular screening in youth—not just for athletes, but for all young individuals. Time constraints during routine evaluations also pose a significant barrier, as providers often have limited opportunities to conduct thorough assessments within the typical clinical workflow. Additionally, state-mandated screening protocols vary widely, which can lead to disparities in how the tool is implemented across different regions.
To address these challenges, we need to prioritize education and awareness among providers, ensuring they understand the critical role of cardiovascular screening in detecting potential risks early. Integrating the screening elements into electronic health record systems can help facilitate more efficient implementation and make it easier to incorporate into routine visits. Beyond that, fostering collaboration between healthcare organizations, schools, and policymakers can promote standardized screening approaches that extend beyond just athletes and encompass all youth, ensuring a broader focus on preventive heart health.
Q: In your research, you also discussed measures of secondary prevention, including Cardiac Emergency Response Plans. In December 2024, the bi-partisan HEARTS Act was signed into law, ensuring that AEDs are available in schools and childcare centers and that students, staff, and sports volunteers receive CPR and AED training. A federal grant program will be established to support these efforts, making sure schools can access the funding they need to implement these life-saving measures. How would you advise school leaders who are looking to implement a new training program on campus? What elements are critical to a CERP?
Implementing an effective Cardiac Emergency Response Plan (CERP) is essential for ensuring the safety of students and staff. School leaders should prioritize several key elements, including ensuring AED devices are accessible, strategically placed and readily available within a short retrieval time; providing comprehensive CPR and AED training, which should extend beyond staff to include students and sports volunteers; and establishing clear emergency response protocols, outlining specific roles and responsibilities in the event of a cardiac emergency.
With the recent passing of the HEARTS Act, schools now have additional support to access funding for life-saving equipment and training. I would advise school administrators to leverage these resources and partner with local healthcare providers or emergency response teams to develop a tailored and effective emergency response strategy. Regular drills and ongoing training are crucial to ensuring that everyone is prepared to act quickly and effectively in an emergency.
Q: Additionally, you recently spearheaded a new initiative with a local high school to provide cardiac screenings for student athletes. What inspired you to provide this program for local youth? How would you advise colleagues at other hospitals across the United States who may be interested in developing a similar program for students?
Our cardiac screening program at Staten Island University Hospital, supported by the Protecting One Young Heart at a Time Foundation, was established in memory of Frank Reali III, who passed away from hypertrophic cardiomyopathy. Since its inception, we have screened thousands of students across 10 Staten Island schools, most recently partnering with Monsignor Farrell High School. Through these efforts, we have identified a total of sixteen cases of serious heart conditions that may have otherwise gone undetected, underscoring the critical importance of early cardiac evaluation.
Beyond our local efforts, I am involved in broader initiatives such as Heart Screen New York, a collaboration between medical professionals from Northwell Health and other leading institutions, alongside foundations like the Louis J. Acompora Memorial Foundation and the Dominic A. Murray 21 Memorial Foundation. These partnerships aim to expand access to cardiac screenings and raise awareness of the importance of early detection across New York State.
For colleagues interested in developing similar programs, collaboration is essential. Partnering with schools, securing funding, and building a dedicated multidisciplinary team—including cardiologists, sonographers, and medical trainees—are key to success. The positive response from students, parents, and school staff highlights the program’s impact in providing peace of mind and potentially life-saving early detection.
Q: Regarding your own career path, could you share your clinical background? What inspired you to pursue pediatric cardiology? Additionally, what spurred you to focus upon cardiac health of young athletes?
Pediatric cardiology has always been a passion of mine because it offers a unique opportunity to positively affect the lives of children and their families. Diagnosing and managing congenital and acquired heart conditions from infancy through adolescence is both challenging and rewarding, allowing me to help shape long-term health outcomes for my patients.
My focus on young athletes stems from both personal and professional interests in preventive cardiology. As a long-distance runner, I understand the importance of maintaining heart health while pursuing sports. Sudden cardiac arrest in athletes is a rare but devastating event, and I am committed to ensuring that young individuals can safely participate in the activities they love. Through education, screening, and advocacy, we can help prevent these tragedies and foster a culture of heart health awareness within our communities.
Q: Over the past few years, the AHA introduced and developed the Nation of Lifesavers™ initiative to empower teens and adults to perform hands-only CPR. Why is it important for families to be trained in CPR and AED use?
The importance of CPR and AED training cannot be overstated. Sudden cardiac arrest can happen anywhere, and survival rates drop significantly with each passing minute without intervention. Immediate bystander CPR and AED use can more than double the chances of survival, making it critical for families to be equipped with these life-saving skills.
The American Heart Association’s Nation of Lifesavers initiative is an excellent step toward ensuring that more individuals are trained to respond in emergencies. Encouraging widespread training in schools and community settings empowers people to take action confidently and can make a significant difference in saving lives. Families should view CPR training not only as a valuable skill but as an essential part of their preparedness for emergencies.
Q: Lastly, do you have any additional reflections to share with health providers or families within our communities regarding either cardiac screenings or CPR training?
If there is one key takeaway from my work in this area, it’s that prevention and preparedness are crucial when it comes to cardiac health. While routine cardiac screenings can help identify potential risks, they are just one part of a comprehensive approach to heart health. It’s equally important for primary care providers to engage in thoughtful discussions with families about heart health and to recognize warning signs such as unexplained fainting or chest pain during exertion.
Even with careful evaluation, cardiac emergencies can still occur, which is why CPR and AED training should be a priority for families, schools, and communities. Empowering individuals with the knowledge and skills to respond effectively in an emergency can truly save lives.
For healthcare providers, fostering an open dialogue with families about heart health and encouraging proactive measures can make a significant impact. For families, staying informed and advocating for heart-healthy lifestyles, along with being prepared for emergencies, plays a vital role in ensuring the well-being of their children. Ultimately, a combination of awareness, prevention, and readiness is key to keeping our youth safe and healthy.
Routine Pediatric CPR Training Can Help Improve Outcomes
The mission of the AHA is to ensure that as many people are trained to provide CPR as possible, thereby increasing the number of survivors with a favorable neurological outcome. Healthcare providers can benefit from a low-dose, high-frequency training model to keep their pediatric CPR skills current.
About Robert Spencer, MD
Dr. Robert Spencer is a board-certified pediatric cardiologist at Staten Island University Hospital, Northwell Health, with a special focus on the prevention of sudden cardiac death in young athletes. He serves as the Director of the Pediatric Simulation Program, where he leads educational initiatives to enhance emergency preparedness among pediatric trainees.
Dr. Spencer earned his medical degree from NYU Langone School of Medicine and completed his pediatric residency at Mount Sinai’s Kravis Children’s Hospital. He pursued his pediatric cardiology fellowship at Columbia University Medical Center.
Beyond his clinical practice, Dr. Spencer is actively involved in community outreach, leading cardiac screening initiatives for students across Staten Island. His efforts have resulted in the identification of previously undiagnosed cardiac conditions, helping to safeguard the health and well-being of young individuals. He has published in peer-reviewed journals and frequently presents on topics related to sudden cardiac death prevention and pediatric cardiac care.
Dr. Spencer is passionate about educating both healthcare providers and the public on the importance of heart health, CPR training, and early detection strategies. His dedication to advancing pediatric cardiology and improving patient outcomes continues to impact both the medical community and the families he serves.