The American Heart Association’s Get With The Guidelines® (GWTG) program is focused on quality improvement for hospitals. One of the GWTG tools is focused on in-hospital resuscitation. How’s that going at your hospital?
We know you are committed to safe, effective resuscitations, but do you know your survival outcomes? How is your hospital compared to others? Let’s look at a Get With The Guidelines-Resuscitation (GWTG-R) data set from the Midwest.
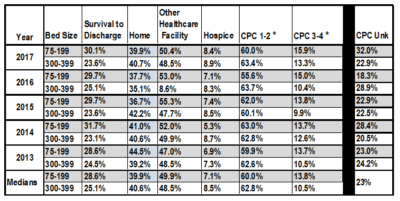
Example of resuscitation outcomes in Midwest hospitals
We published an abstract in Circulation, an American Heart Association scientific journal, examining 6,000 in-hospital cardiac arrests over the past several years where patients were resuscitated.
A commonly reported measure for a successful resuscitation from in-hospital cardiac arrest is survival to discharge. But what does that really tell us? Our study explored an attempt to identify the true condition of those patients at discharge who survived, and their discharge destinations after in-hospital cardiac arrest. In addition to their true outcomes, we explored whether medium or larger sized hospitals have better outcomes.
By using data for the years 2013–2017 from the Get With The Guidelines for 75–199 and 300–399 bed hospitals in the American Heart Association’s Midwest Affiliate, we compared survival to discharge destination and cerebral performance category (CPC) score for patients who survived with and without shockable rhythms.
* Cerebral Performance Category (CPC) Score:
- Good cerebral performance: conscious alert, able to work, might have mild neurologic or psychological deficit;
- Moderate cerebral disability: conscious, sufficient cerebral function for independent activities of daily life, able to work in sheltered environment;
- Severe cerebral disability: conscious, dependent on others for daily support because of impaired brain function, ranges from ambulatory state to severe dementia or paralysis;
- Coma or vegetative state: any degree of coma without the presence of all brain death criteria. Unawareness, even if appears awake (vegetative state) without interaction with environment; may have spontaneous eye opening and sleep/awake cycles, cerebral unresponsiveness;
- Brain death: apnea, areflexia, EEG silence, etc.
In the study above, we not only wanted to show where patients were being discharged to, but what was their neurologic status?
The most revealing data here was that in nearly one-fourth of all cases, neuro status at discharge was not documented. For those that were, however, CPC scores in the 1-2 range were surprisingly high.
Data comparing small and critical access hospitals to larger centers
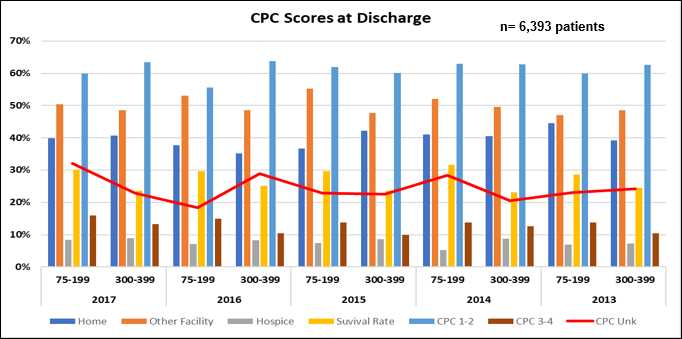
Although survival rates in the 75–199 bed hospitals were always higher, CPC scores were almost always lower for the 300–399 bed facilities, indicating a better neurological outcome. Discharge destinations varied but in almost every case, the majority were sent to other healthcare facilities, such as extended care, skilled nursing, or rehab. A large percentage were discharged home however, verifying again that many patients survived with normal to nearly normal neurological status. Also discovered was that nearly 1 in 4 patients had no CPC score documented at discharge.
It should be noted, although the outcomes from cardiac arrest were better at smaller hospitals, the volume and acuity levels were higher at large hospitals.
Our conclusions
After analyzing hospitals with 75–199 and 300–399 beds, the data showed higher rates of survival to discharge in the smaller hospitals. However, neurologic outcomes were better at larger facilities. This led us to conclude that survival rate alone may not be the most appropriate measure of a successful resuscitation. CPC score at discharge is another key component that should be considered as an indicator of the patient’s condition.
Benchmarking data as we’ve done in this abstract – by region, hospital type, hospital size, and more – helps hospitals hone in on the metrics that truly impact patients’ lives and the quality of care. This is a great example of how GWTG-R can be used to drill down into a question or problem.
We are so pleased to now offer GWTG-R as an integrated program with the RQI 2020 program. Two strong quality programs with one focus – to save more lives. The impact could be life changing.
Art Miller, RN/EMT-P, is a Quality & Systems Improvement Director at the American Heart Association.